Abstract
Background: Venous thromboembolism (VTE) is a major health concern with significant morbidity and mortality. Patients who are hospitalized with acute medical illnesses may have a greater risk for VTE during hospitalization and for several weeks to months after discharge from the hospital. Prophylactic anticoagulant therapy has been shown to reduce such risk. This study evaluated the risk for VTE and the receipt of VTE prophylaxis among patients with or without renal disease who were hospitalized for acute medical illness in the United States (US).
Methods: In this retrospective claims analysis, acutely medically ill patients were identified from the MarketScan databases between January 1, 2012 to June 30, 2015 (index identification period). Patients who were hospitalized with acute medical conditions of cancer, heart failure, infectious diseases, ischemic stroke, respiratory diseases and rheumatic diseases were included in the study population. The first of such hospitalization to occur during the index identification period was defined as the index hospitalization. Patients were further required to have continuous insurance coverage for 6 months prior to (baseline period) and after (follow-up period) the index hospitalization. Patients were grouped into two study cohorts based on whether they had any diagnosis of renal disease (yes vs. no) during the baseline period. The proportion of patients receiving VTE prophylaxis was evaluated. The proportion of patients with a VTE event during the index hospitalization or follow-up period was also evaluated. Multivariate logistic regression analysis was used to determine the impact of renal disease (yes vs. no) on the receipt of VTE prophylaxis. The risk for VTE following the index admission was evaluated by Kaplan-Meier analysis.
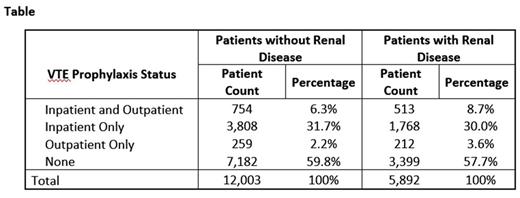
Results: Of patients hospitalized for an acute medical illness (n=17,895; 55.4% female), 32.9% (n=5,892) had renal disease during the baseline period, while 67.1% (n=12,003) had no renal disease. The mean age was higher among patients with vs. without renal disease (64 vs. 56 years, p<0.0001). The mean index hospital length of stay was longer among patients with vs. without renal disease (6.0 vs. 4.2 days, p<0.0001). Approximately 8.7% (n=513) and 6.3% (n=754) of patients with vs. without renal disease received both inpatient and outpatient VTE prophylaxis. Of patients with vs. without renal disease, 57.7% (n=3,399) and 59.8% (n=7,182) did not receive any VTE prophylaxis (Table). After multivariable regression was used to adjust for patient characteristics, patients with renal disease were shown to be less likely to have received any (outpatient or inpatient) VTE prophylaxis (odds ratio: 0.827, confidence interval (CI) [0.771-0.887]; p<0.0001) compared to those without renal disease. The proportion of patients with a VTE event during the index hospitalization was 2.8% (n=165) and 1.3% (n=156) for patients with vs. without renal disease, respectively (p<0.0001). Among patients with vs. without renal disease, 3.5% (n=205) vs. 2.5% (n=304) had a VTE event in the follow-up period after hospital discharge (p<0.0001). The risk for VTE remained elevated for up to approximately 30-40 days after the index hospitalization regardless of renal disease status.
Conclusions: In this real-world study, the risk for VTE remained elevated for patients hospitalized with acute medical illness and, after adjusting for key patient characteristics, patients with baseline renal disease had a higher rate of inpatient and outpatient VTE compared to patients without renal disease. The majority of patients, however, did not receive any VTE prophylaxis. Patients with baseline renal disease had an even lower likelihood of receiving any VTE prophylaxis suggesting an unmet medical need in this population.
Amin: Portola Pharmaceuticals, Inc: Consultancy. Neuman: Portola Pharmaceuticals, Inc: Employment. Lingohr-Smith: Novosys Health: Employment. Menges: Novosys Health: Employment. Lin: Bristol-Myers Squibb: Consultancy; Novosys Health: Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal